The results were found using a 1-hour
pad test to detect any leakage, pelvic floor muscle (PFM) strength testing and
quality of life (QoL) questionnaire. Both methods were found to be similarly
effective in all the parameters tested. The figures below show the relatively
similar effects of both treatments when taking into account the
pre-intervention and post-intervention values.
Since no adverse effects were
observed, the study concluded that the two approaches could be
applied effectively in the treatment of USI. The clinical significance of these
results applies to the way in which practitioners can treat their USI patients.
Therapists can decide whether to use IFT or Biofeedback based on their personal
preference, clinical experience and patient preferences with the confidence
that both methods are effective. The advantages of IFT are its ease of usage
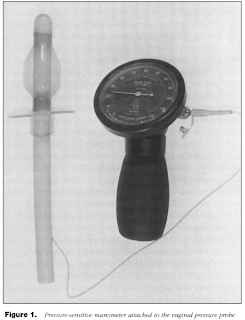
and external application. The Biofeedback treatment may be avoided due to the
relative invasiveness of the vaginal probe required.
At the end of the study, participants
were recommended to perform an at-home program of Kegel exercises, to be
followed up on at a later date. The results of this follow-up survey are yet to
come, but would provide an interesting prognosis of the condition after each
mode of treatment.
The advantages of this study were
that it involved a relatively large sample size and significant intervention
time. The disadvantage was that all participants were female.
The following points summarize the
findings of the literature on Interferential Therapy for Urinary Stress
Incontinence. Electrode placement for IFT is more effective when the anterior
electrode is above the pubic bone, as per the Dumoulin method [2]. IFT was found to be effective in
increasing PFM strength and Quality of Life and also reduced the frequency of
incontinence, volume of urine loss [3][4]. Additionally, IFT was
shown to be better suited to mild and moderate than severe USI [5].
Dosages, Precautions &
Contraindications
To summarize the blog, the following
information can be used to safely apply IFT in a clinical setting:
In order to treat the PFM the following
dosage parameters are recommended: a Phase Duration of 125ms, a current of 80
mA or to patient comfort and a frequency of 2–4000 Hz with an interference
current of 50 Hz.
An important precaution specific to IFT is
the presence of skin conditions as the suction cups may cause irritation or
further damage. Such conditions include thin, frail skin, open wounds or
lesions. Also if the patient is taking anticoagulant medication or is prone to
bruising, this may lead to visible marks where the suction cups had been.
A contraindication specific to IFT for the
PFM is pregnancy due to the inherent electrode positioning of the treatment.
We hope you have enjoyed this blog and
found it relevant to your practice.
References
1.
Demirturk,
F., Akbayrak, T., Karakaya, I. C., Yuksel, I., Kirdi, N., Demirturk, F., Kaya,
S., Ergen, A., Beksac, S. (2008). Interferential current versus biofeedback
results in urinary stress incontinence. Swiss
Medical Weekly, 138(21-22), 317-321.
2.
Dumoulin, C., Seaborne, D. E.,
Quirion-DeGirardi, C. & Sullivan S. J. (1995). Pelvic-floor rehabilitation,
part 1: comparison of two surface electrode placements during stimulation of
the pelvic-floor musculature in women who are continent using bipolar
interferential currents. Journal of the
American Physical Therapy Association, 75(12), 35-42.
3.
Dumoulin, C., Seaborne, D. E.,
Quirion-DeGirardi, C. & Sullivan S. J. (1995). Pelvic-floor rehabilitation,
part 2: pelvic-floor reeducation with interferential currents and exercise in
the treament of genuine stress incontinence in postpartum women – a cohort
study. Journal of the American Physical
Therapy Association, 75(12), 44-49.
4.
Oh-oka, H. (2008). Efficacy of
interferential low frequency therapy for elderly wet overactive bladder
patients. Department of Urology Kobe
Medical Center Japan, 24(2), 178-181.
5.
Turkan, A., Inci, Y. &
Demirturk, F. (2005). The short-term effects of physical therapy in different
intensities of urodynamic stress incontinence. Gynecologic and Obstetric Investigation, 59(1), 43-48.