As with all
bioinstrumentation, a foundation of knowledge of the literature is needed
before applying these methods to patients. The validity of Interferential
Therapy (IFT) as a form of treatment for Urinary Stress Incontinence (USI) was
found by critically reviewing 5 studies, the fifth of which will be discussed
in a later post.
1. Electrode Placement
Methods = Dumoulin et al. (Part 1) [1]
This study compared two IFT electrode
placement methods to maximally stimulate the PFM. Both methods involve a
posterior electrode above the anus; Laycock and Green[3] then
suggest an anterior electrode on the clitoral region and Dumoulin[2]
suggest the anterior electrode should be above the pubic symphysis. A diagram
of these configurations can be seen below. Bipolar electrode placement was used
as it was shown to be equally effective, and because of its ease of
application.
A 2-group crossover design was used,
involving 10 continent women randomly assigned to 2 study groups, each
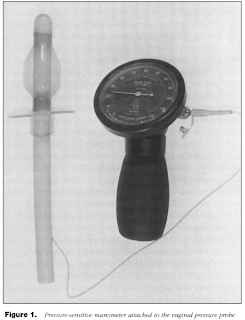
receiving both treatments in random order. The force of PFM contraction was
measured using a vaginal pressure probe attached to a manometer, seen in the
figure below. No difference in pressure was found between the two methods of
electrode placement; however, the Dumoulin method required less current
amplitude to achieve the same pressure and was better tolerated by the
subjects. The study concluded that greater pressures could be more comfortably
reached using the Dumoulin method.
The advantage of this trial was that it
was randomized. The disadvantages were that it involved only a small and
specific sample population of women who did not suffer from incontinence and it
tested the bipolar electrode pattern rather than the conventional quadripolar
pattern. It’s important to note that this study was to develop treatment
guidelines for the following study on postpartum women.
2. Postpartum Women =
Dumoulin et al. (Part 2) [2]
This trial examined 8 postpartum women who’d suffered from USI for
over 3 months after delivery. Treatment included pelvic floor reeducation for 9
half hour sessions combining IFT and pelvic-floor muscle (PFM) exercises. 5
subjects became continent and conditions improved for the other 3. After the
intervention the PFM strength was greater and the volume of urine loss and frequency
of incontinence were lower after the intervention. A 1-year follow-up survey
found these results to remain consistent.
The advantage of this trial was that it involved a significant
intervention time. The disadvantages were that it used only a small and specific
sample population of women and it mixed 2 modes of treatment rather than
determining the most effective.
3. Elderly Overactive Bladder Incontinence = Oh-oka [4]
The focus of this study was the ability of IFT to inhibit detruser
muscle contraction. This muscle is responsible for activating the urge to empty
one’s bladder. Therefore an overactivity of this muscle results in a form of
incontinence known as overactive bladder (OAB).
80 elderly patients between the ages of 69 to 78 years with OAB
incontinence were given 3 months of IFT. The frequency of incontinence and
volume of urine loss were reduced and improvements were seen in the quality of
life questionnaires related to a greater average time spent outdoors. These
effects were seen after an average of 8 sessions and the improvements were
found to last 3 months post-intervention.
The advantages of this trial were that it examined a large sample
population over a relatively long time and conducted a follow-up study to
determine the longevity of the treatment effects. The disadvantage was that it
focused on overactive bladder incontinence that is relevant to, but not exactly
USI.
4. Comparing Different USI
Severity = Turkan et al. [5]
This study examined the effectiveness of
IFT with Kegel exercises in treating patients with different intensities of
USI. 48 patients were assigned to 3 study groups according to the severity of
their USI and were given 15 sessions over 5 weeks. The results showed that the
number of pads used per day, voiding frequency and leakage decreased while the
PFM strength and QoL increased. 88% of the mild USI group and 18% of the
moderate group were cured of their condition while none of the severe group showed
a cured effect, indicating that IFT treatment is better suited to mild and
moderate than severe USI.
The advantage of this trial was that it
used a relatively large sample population. The disadvantage was that it
combined IFT with Kegel exercises rather than focusing primarily on IFT, or
comparing the two treatments.
References
1.
Dumoulin, C., Seaborne, D. E.,
Quirion-DeGirardi, C. & Sullivan S. J. (1995). Pelvic-floor rehabilitation,
part 1: comparison of two surface electrode placements during stimulation of
the pelvic-floor musculature in women who are continent using bipolar
interferential currents. Journal of the
American Physical Therapy Association, 75(12), 35-42.
2.
Dumoulin, C., Seaborne, D. E.,
Quirion-DeGirardi, C. & Sullivan S. J. (1995). Pelvic-floor rehabilitation,
part 2: pelvic-floor reeducation with interferential currents and exercise in
the treament of genuine stress incontinence in postpartum women – a cohort
study. Journal of the American Physical
Therapy Association, 75(12), 44-49.
3.
Green, R.
J. & Laycock, J. (1990). Objective methods for evaluation of interferential
therapy in the treatment of incontinence. IEEE
Transactions on Biomedical Engineering, 37(6), 615-623.
4.
Oh-oka, H. (2008). Efficacy of
interferential low frequency therapy for elderly wet overactive bladder
patients. Department of Urology Kobe
Medical Center Japan, 24(2), 178-181.
5.
Turkan, A., Inci, Y. &
Demirturk, F. (2005). The short-term effects of physical therapy in different
intensities of urodynamic stress incontinence. Gynecologic and Obstetric Investigation, 59(1), 43-48.

Thanks - this is strong work - CY
ReplyDeleteThere's a new treatment for stress incontinence to cause stem cells to generate new healthy tissue. The procedure is called o-shot which has been very effective with my patients.
ReplyDeleteMore can be seen at OShot.info
Hope this helps.
Charles Runels, MD